Jazzy
 Case Background
Case Background
Age: 13 years
Sex: Male, castrated
Breed: Miniature Schnauzer
Weight: 7.4 kg
Reason for visit: Coughing
Medications: Jazzy is currently receiving Heartgard® Plus and Frontline®. He is not on any other chronic medications.
 Clinical History
Clinical History
Please review Jazzy’s clinical history.
Attitude/demeanor: Seemed normal until 24 hours ago.
Coughing: Has been coughing daily for the past 2 to 3 weeks. Cough seems dry but might occasionally be productive (retch at end of cough with swallowing).
Abnormal respirations: Tachypnea and respiratory distress. Owner reports rapid breathing recently and “trouble breathing” over the past 24 hours which prompted the veterinary examination.
Exercise tolerance: Has been slowing down, but was still taking short walks.
Sleep patterns: Has seemed restless at night over the past week with some coughing.
Weight change (loss or gain): Possibly, some mild weight loss.
Appetite: No change.
Usual diet: Purina One® with some table scraps and cold cut treats.
Vomiting: None – occasional retch after cough but nothing produced.
Diarrhea: No.
Syncope: No.
Change in urinary habits: No.
Change in drinking habits: Been drinking more past few days.
Other symptoms or signs: Occasionally scratches ears.
 Physical Exam - General
Physical Exam - General
Please review the results of Jazzy’s physical exam.
Body condition: Good, BCS 4/9.
Attitude: Alert, somewhat anxious.
Mobility | gait: Normal gait upon inspection.
Posture: Standing or sitting.
Hydration: Suspect mild dehydration.
Body temperature: 100.3 F
Arterial pulse – rate, regularity, intensity: 142 beats/min, regular, normal strength.
Respiratory rate & effort: 40, mild inspiratory effort.
Mucous membranes – color & CRT: Pale to pink / 3 seconds.
Jugular venous pulse & pressure: Normal.
Abdominal palpatation: Liver is palpably enlarged; moderate-size bladder.
Lymph nodes: Normal.
Oral cavity: Mild dental calculus, no periodontal disease.
Other abnormalities: Slight odor from ears.
 Physical Exam - Auscultation
Physical Exam - Auscultation
 Physical Exam - Differential Diagnosis
Physical Exam - Differential Diagnosis
- High (could explain most or all of the signs)
- Possible (less likely to explain most of the signs)
- Unlikely
 Diagnostic Test Selection
Diagnostic Test Selection
 Blood Pressure
Blood Pressure
Diastolic blood pressure: Not available for this case
Mean blood pressure: Not available for this case
 Radiography
Radiography
Please review Jazzy’s thoracic radiographs
Click here for Jazzy’s radiograph viewer (measure VHS and VLAS here) View the right lateral radiograph
 Clinical Labs
Clinical Labs
Please review Jazzy’s lab results
Serum chemistriesBUN: 38 mg/dL Normal: <30 mg/dL
Creatinine: 1.8 mg/dL Normal: 0.3 – 2.1 mg/dL
Sodium: 149 mEq/dL Normal:138 – 154 mEq/dL
Potassium: 3.7 mEq/dL Normal: 3.6 – 5.2 mEq/dL
Chloride: 112 mEq/dL Normal: 105 – 119 mEq/dL
ALT: 32 IU/dL Normal: <75 IU/dL
ALP: 56 IU/dl Normal: <100 U/dL
Glucose: 104 mg/dL Normal: 68 – 126 mg/dLHeatworm
Heartworm test results: NegativeUrinalysis
Urinalysis – USG: 1.024
Urinalysis – protein: Trace
Urinalysis – biochemical: All values within normal limits
Urinalysis – sediment evaluation: Occasional epithelial cells limitsCBC
White blood cells: All values within normal limits
Red blood cells: Hb – 13.4 G/L; PCV – 40.1%
Platelets: 272,000
 Echocardiography
Echocardiography
Please review the results of Jazzy’s echo
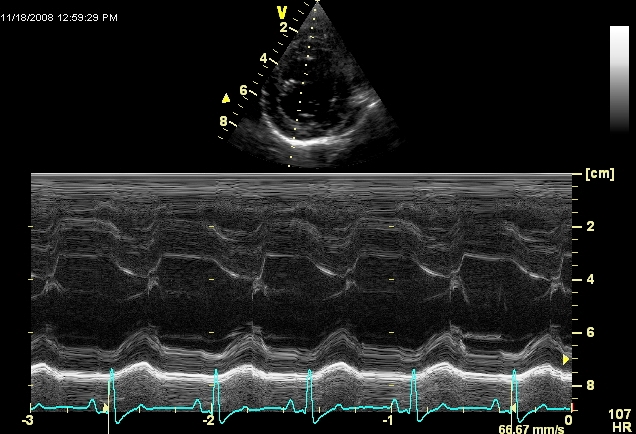
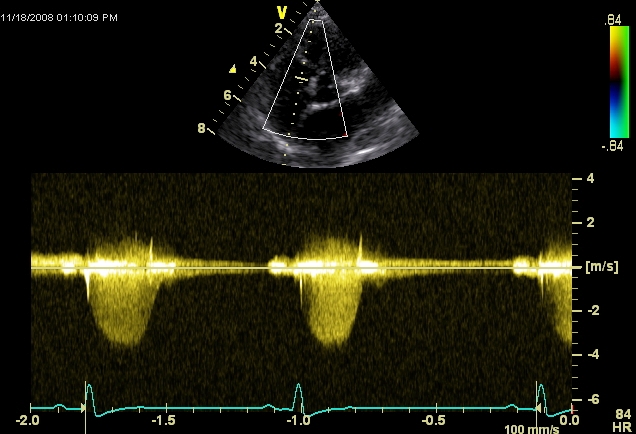
Watch echo #1The echo diagnosis is mitral and tricuspid regurgitation due to chronic degenerative valve disease with secondary left heart enlargement. There are selected images shown. The right parasternal long axis (#1) shows a prolapsing mitral valve with subjective enlargement of the left atrium and ventricle. The short-axis image (#2) shows a hyperdynamic and subjectively dilated left ventricle. The third image is an apical image centered on the left ventricle (top) and atrium (bottom). The mitral valve is thick and prolapses (anterior leaflet). The color Doppler echocardiogram (#4) is another apical view that shows an eccentric jet of mitral regurgitation (coded in green). The M-mode study showed left ventricular dilation for the size of the dog and a normal fractional shortening. The septal excursion is greater than free wall, typical of volume overload of the left ventricle. The mitral Doppler shows a holosystolic jet of regurgitation. The tricuspid Doppler shows a holosystolic jet of tricuspid regurgitation; the maximal velocity is <3 m/s indicating an absence of significant pulmonary hypertension.
 ECG
ECG
Please review Jazzy’s ECG.
Click here for Jazzy's 6 - lead ECG Technical quality, leads, paper speed, calibrations: Satisfactory recording; 6 frontal leads and lead 2 rhythm strip recorded; paper speed 50 mm/sec; calibration 5 mm/mV
Artifacts: None
Heart rate: 180/min
Rhythm – regular or irregular | patterns: Regular
Heart rhythm disturbances: Sinus tachycardia; although auscultated (see Auscultation), no premature complexes were detected during this recording
P wave abnormalities – morphology, amplitude, duration: Slightly wided (0.55 sec) especially evident in lead III (P-mitrale); normal amplitude (appear smaller due to calibration factor)
QRS abnormalities – axis, morphology, amplitude, duration: Normal frontal axis, upper limit duration, increased voltages (deep Q-waves with 4.8 mV R-waves in lead II suggestive of eccentric LV hypertrophy or dilatation)
Abnormal intervals – PR, QRS, QT: Normal intervals
Other: Slurred ST segment
 Diagnosis
Diagnosis
You’re ready to form a diagnosis for Jazzy! Which of the following diagnoses are correct (you can select more than one)?
Click here to learn more about the stages of heart disease (ABCD Brochure)
 Initial Therapy
Initial Therapy
The following are typical treatments for severe left-sided CHF:
 Treatment - Long Term Therapy
Treatment - Long Term Therapy
You’re ready to form a treatment plan for Jazzy!
 Follow Up
Follow Up
5 Month follow up: Jazzy was re-examined 5 months later and has been doing well. Kidney function was stable at that examination. Repeated thoracic radiographs showed progressive cardiomegaly, but relatively clear lung fields. Click here to view 5 month left lateral radiograph