Cy
 Case Background
Case Background
Name: Cy
Age: 7 years old
Sex: Male, neutered
Breed: Domestic shorthair
Weight: 4.5 kg
Reason for visit: Cy presented for sudden onset respiratory distress
Medications: Heartworm prevention
Age: 7 years old
Sex: Male, neutered
Breed: Domestic shorthair
Weight: 4.5 kg
Reason for visit: Cy presented for sudden onset respiratory distress
Medications: Heartworm prevention
 Clinical History
Clinical History
Attitude/demeanor: Anxious
Coughing: No cough
Abnormal respirations: Mild
Exercise intolerance: Unknown
Sleep patterns: No change
Weight change (loss or gain): Mild weight loss
Appetite: Not interested in food the last 18 hours
Usual diet: Name brand adult maintainance
Vomiting: None
Diarrhea: None
Syncope: No
Change in urinary habits: No
Change in drinking habits: No
Other symptoms or signs: None
Indoor/outdoor environment: Indoor
Coughing: No cough
Abnormal respirations: Mild
Exercise intolerance: Unknown
Sleep patterns: No change
Weight change (loss or gain): Mild weight loss
Appetite: Not interested in food the last 18 hours
Usual diet: Name brand adult maintainance
Vomiting: None
Diarrhea: None
Syncope: No
Change in urinary habits: No
Change in drinking habits: No
Other symptoms or signs: None
Indoor/outdoor environment: Indoor
 Physical Exam - General
Physical Exam - General
Body condition: Mildly underweight – BCS 4/9
Attitude: Anxious
Mobility | gait: Normal
Posture: Laying in sternal recumbency, with head up, mild head and neck extension
Hydration: Normal
Body temperature: 98.3 F
Arterial pulse – rate, regularity, intensity: 230, irregularly irregular, variable strength
Rate & respiratory effort: 48, mildly increased
Mucous membranes – color & CRT: Pale pink, 2 seconds
Jugular venous pulse & pressure: Normal
Abdominal palpitation: Normal, moderate size bladder
Lymph nodes: Normal
Oral cavity: Normal
Other abnormalities: None
Attitude: Anxious
Mobility | gait: Normal
Posture: Laying in sternal recumbency, with head up, mild head and neck extension
Hydration: Normal
Body temperature: 98.3 F
Arterial pulse – rate, regularity, intensity: 230, irregularly irregular, variable strength
Rate & respiratory effort: 48, mildly increased
Mucous membranes – color & CRT: Pale pink, 2 seconds
Jugular venous pulse & pressure: Normal
Abdominal palpitation: Normal, moderate size bladder
Lymph nodes: Normal
Oral cavity: Normal
Other abnormalities: None
 Physical Exam - Auscultation
Physical Exam - Auscultation
Listen to Cy’s heart- located over the sternally over the ventral thorax.
(Recommend high-end headphones)
Which of the following finding(s) are present based on your auscultation? Choose all correct options.
 Physical Exam - Differential Diagnosis
Physical Exam - Differential Diagnosis
The following are potential diagnosis for you to consider at this time. Based on the history and the physical examination, please indicate the likelihood of each as:
- High (could explain most or all of the signs)
- Possible (less likely to explain most of the signs)
- Unlikely
Hypertrophic cardiomyopathy
Restrictive cardiomyopathy
Primary respiratory disease
 Diagnostic Test Selection
Diagnostic Test Selection
Non-invasive blood pressure
CBC with platelet count
Coagulation profile
Serum biochemical profile (includes electrolytes)
Urinalysis
Serum thyroxine (T4)
Heartworm antigen test
Heartworm antibody test
Heartworm microfilaria test
NT-ProBNP
Cardiac troponin-I
Thoracic radiographs
Echocardiogram doppler studies
ECG rhythm strip or 6 lead ECG
 Blood Pressure
Blood Pressure
Systolic blood pressure: 100 mmHg
Diastolic blood pressure: Not available for this case
Mean blood pressure: Not available for this case Consensus Statements of the American College of Veterinary Internal Medicine (ACVIM) provides the veterinary community with up-to-date information on the pathophysiology, diagnosis, and treatment of clinically important animal diseases. In 2018, ACVIM published updated guidelines for the Identification, Evaluation, and Management of Systemic Hypertension in Dogs and Cats in the the Journal of Veterinary Internal Medicine.Click here to view and download a PDF of the ACVIM consensus statement, guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats.
Diastolic blood pressure: Not available for this case
Mean blood pressure: Not available for this case Consensus Statements of the American College of Veterinary Internal Medicine (ACVIM) provides the veterinary community with up-to-date information on the pathophysiology, diagnosis, and treatment of clinically important animal diseases. In 2018, ACVIM published updated guidelines for the Identification, Evaluation, and Management of Systemic Hypertension in Dogs and Cats in the the Journal of Veterinary Internal Medicine.Click here to view and download a PDF of the ACVIM consensus statement, guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats.
Cy's systolic blood pressure is:
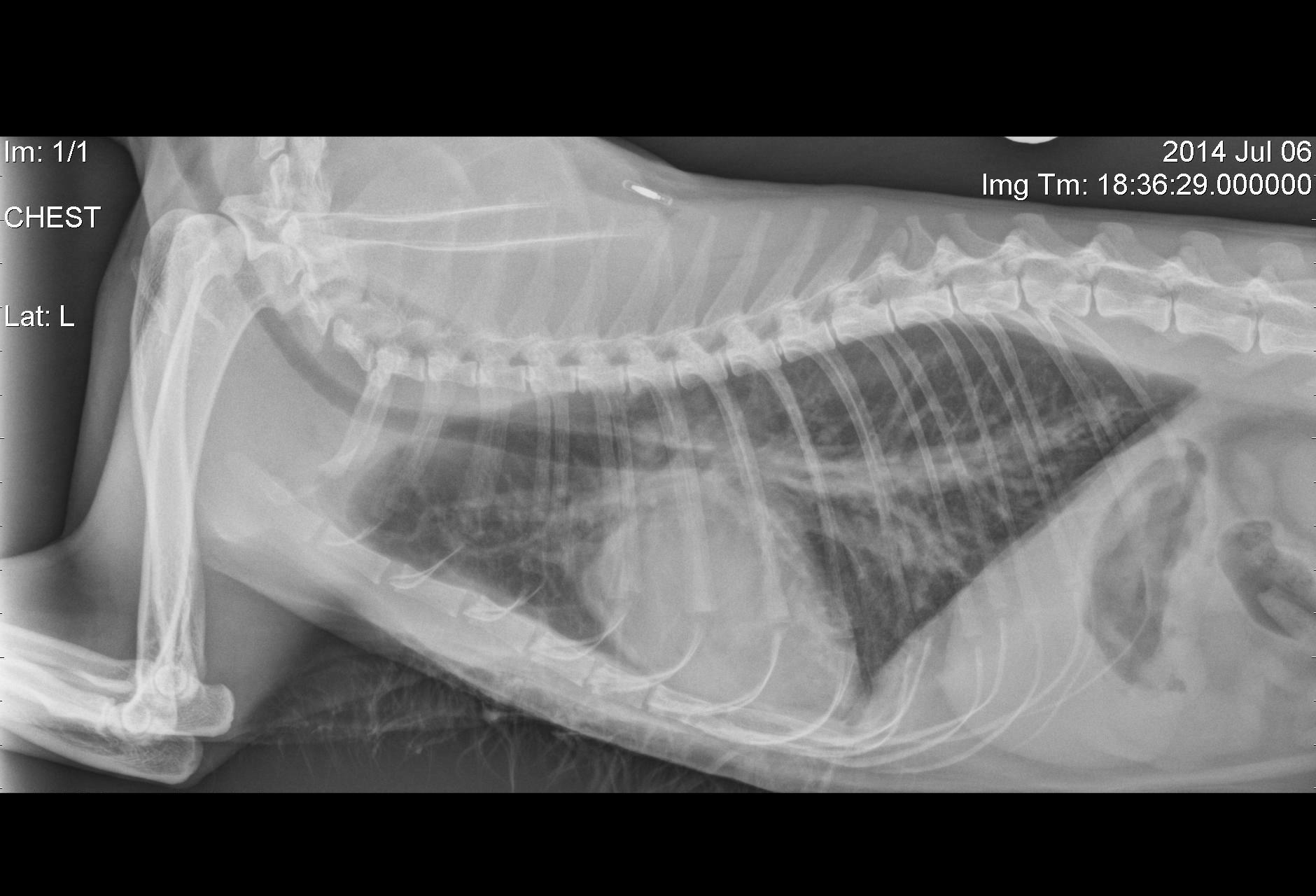
 Radiography
Radiography
Please review Cy’s radiographs
Click here for Cy’s radiograph viewer (measure VHS here) View the right lateral radiograph
Which interpretation is correct?
 Clinical Labs
Clinical Labs
Serum chemistries
BUN: 29 mg/dL Normal: 15-34 mg/dLCreatinine: 2.0 mg/dL Normal: 0.8 – 2.3 mg/dL
Sodium: 152 mmol/L Normal:147 – 156 mm0l/L
Potassium: 4.5 mmol/L Normal: 3.9 – 5.3 mm0l/L
Chloride: 123 mmol/L Normal: 111 – 125 mm0l/L
ALT: 21 U/L Normal: 0 – 62 U/L
ALP: 56 U/L Normal: 28 – 100 U/L
NT-proBNP: Test spot darker than control (270 pmol/L) Normal: <100 pmol/L
Heartworm
Heartworm antibody test results: NegativeUrinalysis
Urinalysis – USG: 1.021Urinalysis – protein: Negative
Urinalysis – biochemical abnormalities: None
Urinalysis – abnormal sediment: None
CBC
White blood cells: 11.3 K/microLRed blood cells: 8.12 M/microL
Platelets: 144 K/microL, scanning reveals clumping with adequate platelet numbers.
 Echocardiography
Echocardiography
Please review the results of Cy’s echo
Watch echo #1The most correct echocardiographic diagnosis is:
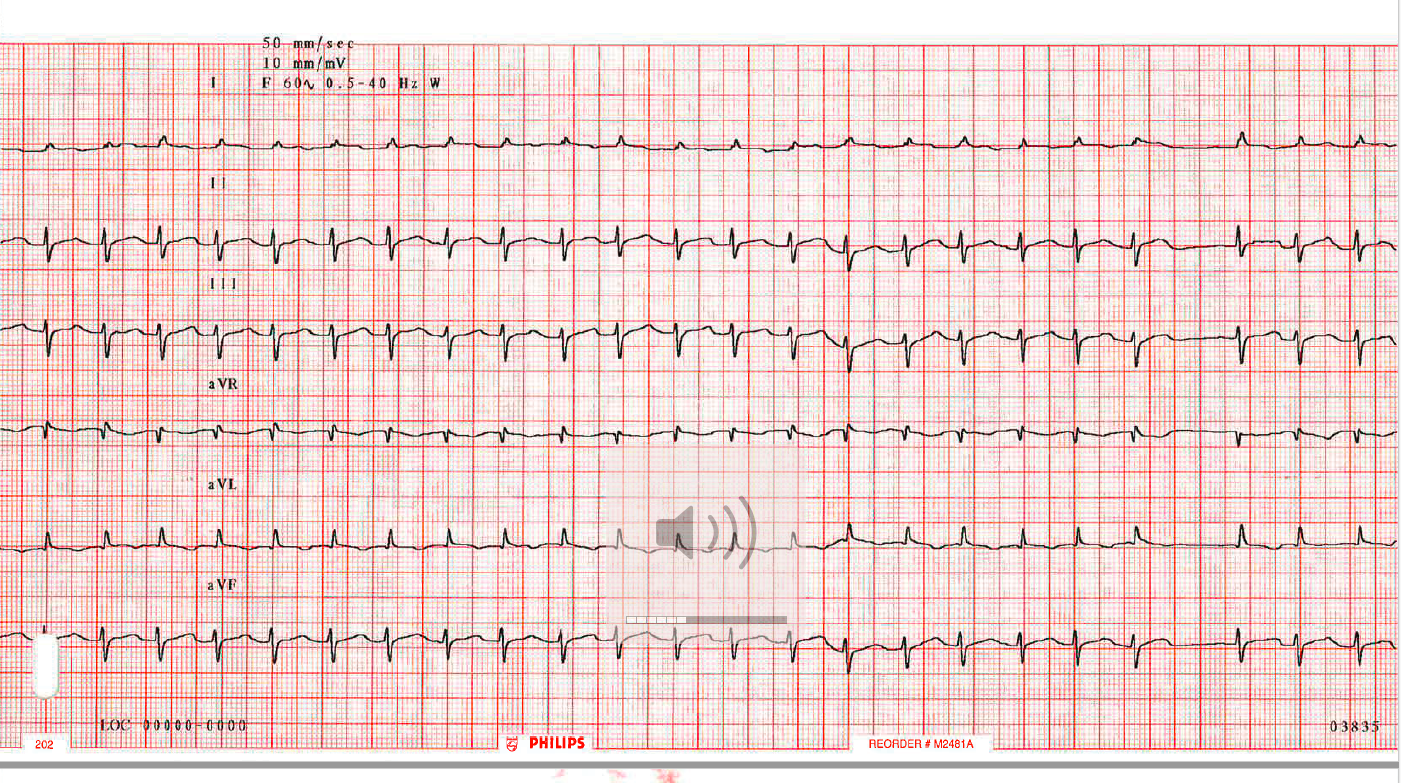
 ECG
ECG
 Diagnosis & Treatment
Diagnosis & Treatment
You’re ready to form a diagnosis and treatment plan for Cy! Please select your answer to each question below.
What kind of heart disease does this cat have?
What treatment(s) would you recommend for Cy?
 Follow Up
Follow Up
Please review Cy’s follow-up visit information
Physical exam: Respiration rate = 26, heart rate = 160 (irregularly irregular)Systolic blood pressure (non-invasive Doppler flow method): Normal, 140 mm HgThoracic radiographs were obtained:
Click here for Cy's right lateral follow up radiograph
The most correct radiographic interpretation is:
 Post Test - CE
Post Test - CE
Please answer the following questions.
The key ECG factors in diagnosis of atrial fibrillation in cats include:
Which of the following is an advantage of pursuing NT-ProBNP testing in a patient with respiratory distress?
- Which of the following causes of pleural effusion would most likely have an abnormal, point of care NT-ProBNP snap test result?
What is the best diagnostic test to identify the type and severity of a cardiomyopathy in a cat with suspected congestive heart failure?
Why would diltiazem be a better choice for treating atrial fibrillation in a congestive heart failure (CHF) feline patient than atenolol?
 RACE Certification
RACE Certification
RACE Certification
Fill out the following form in order to receive your certificate.