Jake
 Case Background
Case Background
Age: 7 years
Sex: Male, neutered
Breed: Doberman
Weight: 35.3 kg (77.7 lbs)
Reason for visit: Annual health evaluation
Medications: Heartworm prevention, fish oil supplementation
 Clinical History
Clinical History
Please review Jake’s clinical history.
Attitude/demeanor: Normal
Coughing: None
Respirations: Normal rate and effort (owner does not count rate)
Exercise tolerance: Normal, walks 3 miles daily with owner
Sleep patterns: Normal, sleeps in bed with owner
Weight change (loss or gain): None according to owner but according to hospital records there is a 0.5 kg increase since the last exam 12 months ago
Appetite: Normal appetite
Usual diet: Purina® OM™, 4 cups per day
Vomiting: None
Diarrhea: None
Syncope: None
Change in urinary habits: None, normal
Change in drinking habits: None, normal
Other symptoms or signs: None, normal
 Physical Exam - General
Physical Exam - General
Please review the results of Jake’s physical exam.
Body condition: Normal, BCS 4.5/9
Attitude: Normal
Mobility | gait: Normal
Posture: Normal
Hydration: Normal
Body temperature: 101.8 F
Arterial pulse – rate, regularity, intensity: 130 beats/min, regular, synchronous, normal amplitude
Respiratory effort: 18 breaths per minute
Mucous membranes – color & CRT: Pink, <1.5 sec
Jugular venous pulse & pressure: Not examined
Abdominal palpatation: Normal
Lymph nodes: Normal
Oral cavity: Normal
Other abnormalities: None
 Physical Exam - Auscultation
Physical Exam - Auscultation
Let’s auscult Jake’s heart & lungs. (Recommend high-end headphones)
Palpitation of the chest wall overlying the heart (precordial palpitation) was normal. Jake’s lung sounds are normal. These heart sounds were heard when the stethoscope was positioned over Jake’s left apex.
 Physical Exam - Differential Diagnosis
Physical Exam - Differential Diagnosis
- High (could explain most or all of the signs)
- Possible (less likely to explain most of the signs)
- Unlikely
 Diagnostic Test Selection
Diagnostic Test Selection
 Blood Pressure
Blood Pressure
Diastolic blood pressure: Not available for this case
Mean blood pressure: Not available for this case Consensus Statements of the American College of Veterinary Internal Medicine (ACVIM) provide the veterinary community with up-to-date information on the pathophysiology, diagnosis, and treatment of clinically important animal diseases. In 2018, ACVIM updated guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats in the the Journal of Veterinary Internal Medicine.
Click here to view and download a PDF of the ACVIM consensus statement, guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats.
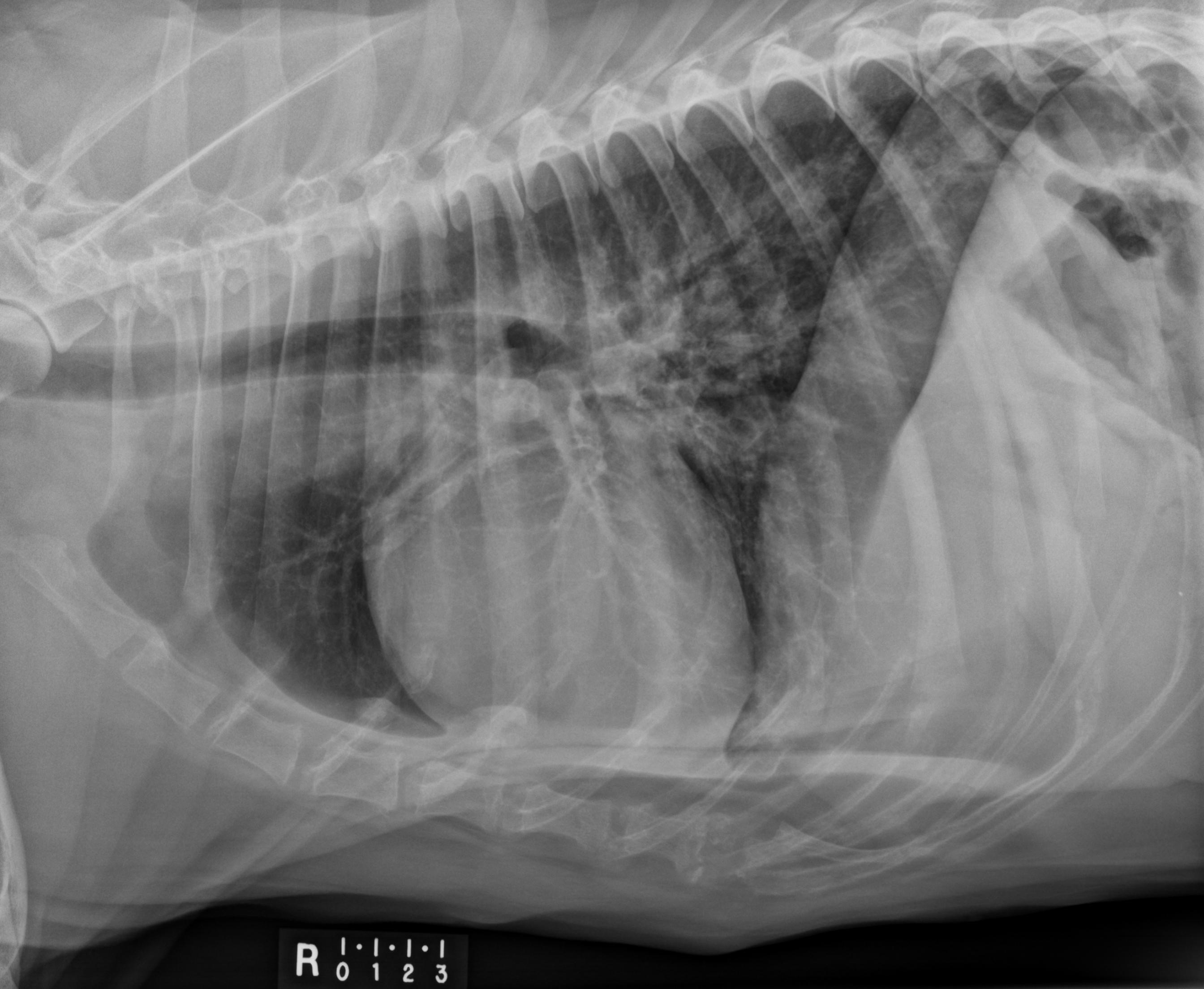
 Radiography
Radiography
 Clinical Labs
Clinical Labs
Please review Jake’s lab results
Serum chemistries
BUN: 14 mg/dL, Normal: 5 – 29 mg/dL
Creatinine: 1 mg/dL, Normal: 0.3 – 2.0 mg/dL
Sodium: 148 mm0l/L, Normal:138 – 154 mm0l/L
Potassium: 3.8 mm0l/L, Normal: 3.6 – 5.2 mm0l/L
Chloride: 114 mm0l/L, Normal: 114 – 126 mm0l/L
ALT: 89 IU/dL, Normal: 10 – 130 U/dL
ALP: 80 IU/dL, Normal: 24 – 147 U/dL
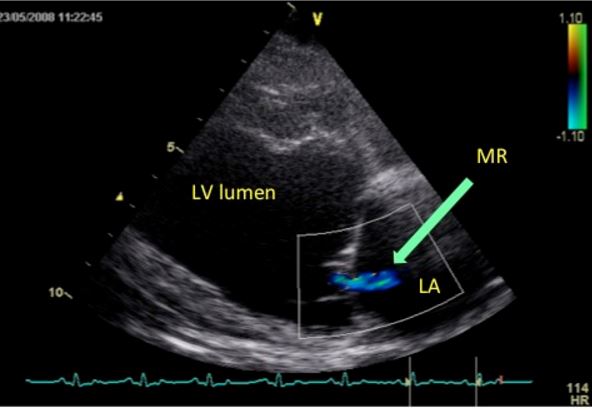
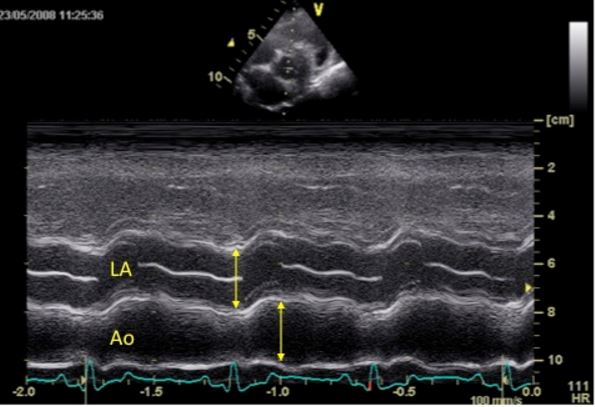
 Echocardiography
Echocardiography
Please review the results of Jake’s echo
Watch echo #1 Subjective – lesions of valves, myocardium, pericardial space: Normal morphology of all valves. Normal myocardial echogenicity.
LV chamber size and thickness: LV dilated. Normal thickness.
Left atrial size: Normal
LVIDd & LVIDs: Increased
LV shortening fraction: Subjectively reduced and measures low at 9.26% (breed specific normal 20-35%).
RA, RV and pulmonary artery: Normal RA, RV and pulmonary artery.
Effusions: None.
Doppler results: Mild mitral regurgitation is documented which is the most likely cause of the murmur. In addition, mild tricuspid regurgitation and pulmonic insufficiency are documented which are normal findings in the majority of dogs and do not result in murmurs.
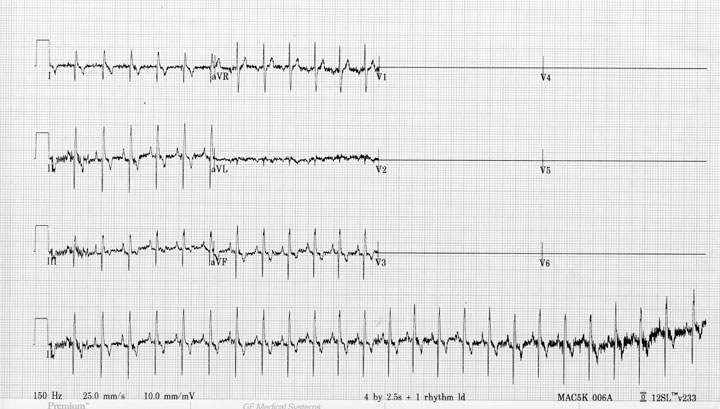
 ECG
ECG
Please review Jake’s ECG
An ECG is not a first priority test for Jake at this time because his rhythm based on auscultation was regular. However, intermittent arrhythmias are common in dilated cardiomyopathy and thus Jake would benefit from a Holter examination (A 24-hour ambulatory ECG). The results of Jake’s Holter can be found below.Click here to view Jake's ECG
Technical quality, leads, paper speed, calibrations: Adequate, 6 lead, 25 mm/sec
Artifacts: Intermittent 60 cycle electrical interference artifact
Rhythm – regular or irregular, patterns: Sinus
Heart rhythm disturbances: None
P Wave abnormalities – morphology, amplitude, duration: None
QRS abnormalities – axis, morphology, amplitude, duration: None
HOLTER EXAMINATION REPORT
Holter duration: 17 hours, 49 minutes
Average HR: 105 bpm
Pauses: # pauses > 3.5 sec = 0
Longest pause: n/a
# Single VPC: 750
# VPC couplets: 1
# VPC triplets: 3
Run of V tach: 1
Longest run of V tach: 6 beats
# Single SVPB: 0
# SVPB couplets: 0
# SVPB triplets: 0
Run of SVT: 0
Longest run of SVT: n/a
SVT HR: n/a
Interpretive summary: The recording quality was good. They underlying rhythm was sinus arrhythmia, sinus tachycardia and sinus rhythm with occasional VPCs. The ventricular arrhythmias overall were not considered severe but are considered complex because repetitive forms (couplets, triplets and short runs of ventricular tachycardia) were noted. These findings are consistent with a diagnosis of DCM in the Doberman.